It is a zoonotic viral infection that is very rare in our part of the world. In 1970, the first human cases were detected in Africa (Democratic Republic of the Congo). Over the past 10 years, the number of cases has risen in other West and Central African countries. Active outbreaks have been reported in several African countries.
On other continents, very few infections have been detected in humans.
In May of 2022 the United Kingdom reported two cases. Since then, many countries in Europe, including Spain, have reported MPX infections.
To date the most common transmission mechanism in humans has been direct or indirect contact, mainly with primates or rodents from endemic areas.
MPX transmission is similar to that of classic (eradicated) smallpox, through large respiratory droplets by direct and prolonged contact, as well as through bodily fluids or fomites.
The risk of transmission is greater when exanthematous lesions develop. The likelihood of transmission depends on the nature and proximity of the contact.
There is an increased risk of infection among cohabitants, sexual partners, other close contacts, and healthcare professionals not using PPE.
The incubation period ranges from 6 to 16 days, but can also range from 5 to 21.

Characteristic symptoms are fever, headache, swollen lymph nodes, lower back pain, muscle pain, and fatigue. A rash subsequently appears, with the areas most affected being the face, palms, and soles of the feet. This rash evolves sequentially into papules, vesicles and scabs. It may take up to some 21 days for the scabs to disappear.
It is very often a self-limiting disease. The most serious cases often occur in children.
The clinical diagnosis is made taking into account the differences with other exanthematous diseases, bacterial skin infections, scabies, syphilis and allergies caused by medications.
The confirmation diagnosis can only be carried out by means of tests carried out at a Microbiology laboratory, via electron microscopy, culture, or PCR. The sample should include skin lesions such as smears of vesicular lesions, exudates or scabs. The most widely available technique at laboratories in general is PCR. Samples of pharyngeal or nasopharyngeal exudate must be obtained for the virus culture (usually only performed at leading state laboratories). With respect to skin biopsies, the samples may be vesicular or pustular lesions.
There is no specific treatment for MPX at this time, only supportive and symptomatic measures.

 Español
Español Português
Português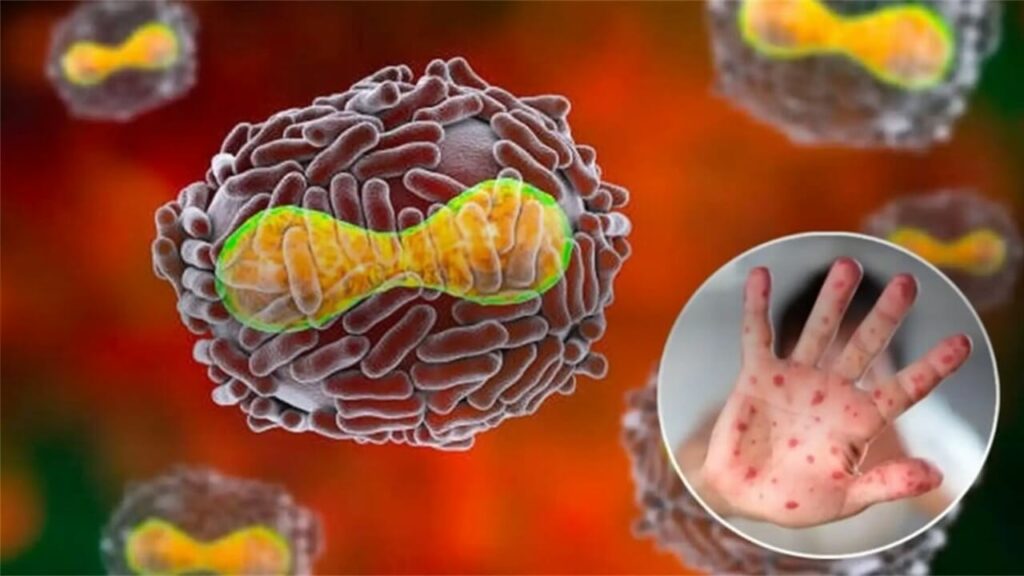
¿Quieres recibir noticias como ésta en tu email?
Suscríbete a la newsletter