The role of the microbiology laboratory is key, providing increasingly faster and more accurate diagnostics
The resistance of bacteria to antibiotics, one of the ten biggest public health threats facing humanity according to the World Health Organisation, is growing at an alarming rate. Data from the Centre for Disease Control and Prevention show that each year in Europe over 670,000 infections are due to antibiotic-resistant bacteria and approximately 30,000 people die as a direct consequence.
“There is even talk of a ‘post-antibiotic era’ in which common infections could become potentially lethal again due to the lack of effective antibiotics”, says Pedro Fernández Echauri, specialist in microbiology at the diagnostics company, Analiza. “The problem is not limited to serious diseases in hospital environments; we are already finding common diseases which are sometimes difficult to treat, for example, gonorrhoea, tuberculosis and pneumonia”, he adds.
The solution requires a multidisciplinary approach to antibiotic resistance from all players in the field of health. The programmes for optimising antibiotic use (PROA) in most Spanish hospitals are playing a decisive role, seeking to improve patient prognosis, control the appearance of resistance and ensure the use of cost-effective treatments. These programmes are coordinated by the infection control committee in each hospital which puts together a multidisciplinary team with three essential professionals – an infectious disease doctor, a pharmacist and a microbiologist- and others, such as disease prevention specialists, intensive care specialists, paediatricians and nursing staff.
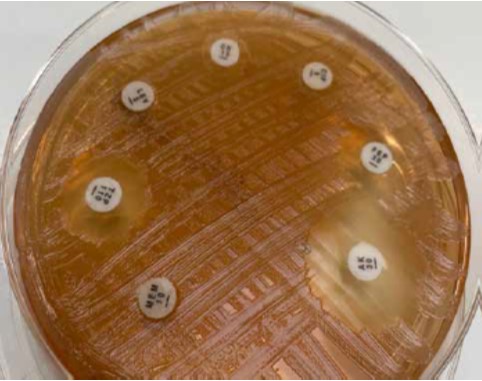
Plate with isolated multi-drug resistant Pseudomonas aeruginosa
Importance of the laboratory
The microbiology laboratory should be the first line of action in this matter according to Mercedes Lerma, specialist in microbiology at Analiza. “Our role is to identify pathogens and determine their antimicrobial susceptibility patterns and resistance, and quickly provide clinical staff with reliable information. We validate and notify the hospital’s infection control team of the existence of multi-drug resistant bacteria”, she says.
The hospital programmes for optimising antibiotic use seek to control the appearance of antibiotic resistance
The infection control team isolates patients who are carriers after being notified by the microbiology laboratory, which also provides doctors with information so they can prescribe the most appropriate directed therapy. “This work is essential because it has been widely documented that patient survival is directly related to rapid identification of the pathogen causing the infection”, explains Fernández Echauri.
The foundations of the clinical laboratory are therefore based on maximising the speed and certainty of diagnostics, using the most advanced techniques and collaborating with the hospital to prevent the dissemination of disease and resistance in wards and among hospitalised patients. Another crucial function of the laboratory, in addition to transmitting its experience and results at a scientific or investigative level is to make society aware of the importance of the rational use of antibiotics, underlines Pedro Fernández Echauri.

 Español
Español Português
Português
¿Quieres recibir noticias como ésta en tu email?
Suscríbete a la newsletter